
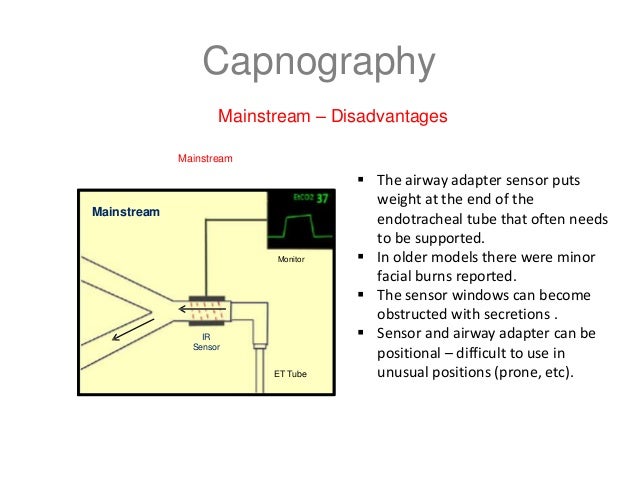
In children, for selecting an endotracheal tube, a variety of formulas and techniques are used to find the endotracheal tube size that minimizes both pressure induced tracheal injury and aspiration potential or variable ventilation. Therefore, it is desirable to intubate trachea with an appropriate but not an oversized endotracheal tube. However, uncuffed endotracheal tube may increase the risk of aspiration and lead to erratic delivery of preset tidal volume during mechanical ventilation. The most important aspect may not be about whether the method is sidestream or mainstream, but that you are monitoring CO2.Uncuffed endotracheal tubes are commonly used in children in an attempt to decrease the potential for pressure induced tracheal injury. Further research may indicate which method is more advantageous to utilize for your specific procedures and situations. Also, when using anesthetic agents, sidestream monitoring needs to have a scavenge system in place to divert the expired and sampled gas safely back into the anesthesia machine so that the room air during the procedure gets contaminated with expired anesthetic agent.īoth methods are acceptable for measuring CO2. The readings may be less accurate because of the variables involved with pulling the sample from the patient to the monitor, then through a water trap, and into the internal sensor. Sidestream CO2 probably has less potential for major parts replacement because the sensor is internal. Industry advancements have made the sensor less vulnerable to damage, but the risk still exists. The disadvantage is the sensor, which is prone to being dropped or damaged and is quite expensive to replace. Mainstream is widely regarded as the more accurate method of measuring CO2 readings. Sidestream CO2 monitoring is widely used throughout clinical applications. The nasal cannulas and sample tubing are usually disposable, and the water trap can be changed out in the event of it becoming clogged or filling with water. The water trap is used to trap the heavier water vapor from entering the monitor, which can cause damage and errant readings. Usually the sample tube first will enter a water trap and/or filter which is attached to the monitor. For this method, the patient’s exhalation air is pulled through a small tube, usually 6-8’ long, from the sample site (usually a nasal cannula or a mask) and into the monitor. Sidestream CO2 uses a sensor that is located inside the monitor instead of an external sensor. The greatest concern with this sensor is that it is susceptible to damage from mishandling, dropping it on the floor, etc. The sensor is corded and connects to the patient monitor and the sensor located at the distal end snaps into an adapter in the airway tubing, mask, etc. This method provides a very accurate reading because since the sensor is at the actual airway, there are far less variable involved that could interfere with an accurate reading (see sidestream summary below). The sample is taken directly from the airway. Mainstream CO2 is measured through the use of a sensor that is inserted via an airway adapter. The measurement is achieved when the sample air passes through an infrared light, which when equipped with the proper detector can provide a measurement for the CO2. Non-Diverting, or having the sensor at the sample site (airway), is the way in which mainstream CO2 is performed. Diverting, or taking the sample gas from the airway and transporting it through a tube to the sensor, is the way in which sidestream CO2 monitoring works. For CO2 monitoring, or Capnography, the method is either “diverting” or “non-diverting”. In this article, we will provide a brief overview of each method. There are two ways to measure CO2 in clinical applications, mainstream or sidestream. This parameter plays an even more prevalent role in the administration of anesthesia. Maybe the single most important reading that can be taken from a patient to truly measure their current physiological state is their expired CO2 measurement.


 0 kommentar(er)
0 kommentar(er)
